Scientists have developed a number of pharmaceutical and non-pharmaceutical interventions to comprise the present coronavirus illness 2019 (COVID-19) pandemic, which is attributable to the speedy outbreak of the extreme acute respiratory syndrome coronavirus 2 (SARS-CoV-2). For instance, the speedy growth of COVID-19 vaccines has been instrumental within the prevention of extreme sickness and deaths worldwide.
In Africa, owing to poor vaccination protection, the depth of extreme an infection and dying as a consequence of SARS-CoV-2 an infection stays excessive. Moreover, the emergence of latest SARS-CoV-2 variants has lowered the efficacy of accessible vaccines and therapeutics, that are based mostly on the spike protein of the unique virus. The World Well being Group (WHO) has categorised these SARS-CoV-2 variants as variants of concern (VOC) and variants of curiosity (VOI).
Research: Unsuppressed HIV an infection impairs T cell responses to SARS-CoV-2 an infection and abrogates T cell cross-recognition. Picture Credit score: Vector-3D / Shutterstock.com
HIV and COVID-19
The impact of COVID-19 in sufferers with human immunodeficiency virus (HIV) shouldn’t be clear. In a single examine based mostly on small pattern dimension, researchers report that individuals dwelling with HIV (PLWH) exhibited comparable COVID-19 outcomes in comparison with wholesome people.
Nonetheless, a bigger epidemiological examine has contradicted the earlier report and recognized elevated hospitalization and dying charges as a consequence of COVID-19 amongst PLWH as in comparison with HIV-negative people.
A earlier examine revealed that extended shedding of excessive titers SARS-CoV-2 and the emergence of many mutations have been present in people with superior HIV and antiretroviral therapy (ART) failure. Scientists have acknowledged that each B-cells and T-cells play essential roles in offering safety towards SARS-CoV-2 an infection.
Curiously, research have proven that T-cell responses can supply safety even within the absence of humoral responses. This means that in a person with inherited B-cell deficiencies or hematological malignancies, T-cells will play an essential function of their restoration from SARS-Cov-2 an infection.
Earlier stories have indicated that COVID-19 severity is said to a weak SARS-CoV-2-specific CD4⁺ T-cell polyfunctionality potential. A number of research have additionally proven that messenger ribonucleic acid (mRNA) vaccines can stimulate Th1 and Th2 CD4+ T-cell responses, which could be correlated with post-boost CD8+ T-cell responses and neutralizing antibodies. Thus, scientists have expressed the necessity for extra insights relating to T-cell-mediated safety towards SARS-CoV-2 an infection.
Concerning the examine
In sub-Saharan Africa, the prevalence of HIV is excessive; Thus, you will need to decide the impact of HIV in people identified with COVID-19. Understanding the illness final result on this affected person inhabitants will assist researchers and policymakers formulate efficient methods to guard them from SARS-CoV-2 an infection.
A brand new examine posted to the medRxiv* preprint server evaluates the influence of HIV an infection on the standard and epitope specificity of SARS-CoV-2 T-cell responses throughout the first and second waves of COVID-19 in South Africa. On this examine, scientists investigated the antigen-specific CD4+ and CD8+ T-cell responses in a cohort of SARS-CoV-2-infected people with and with out HIV an infection.
In, circulate cytometry was used to estimate T-cell responses following peripheral blood mononuclear cell (PBMC) stimulation with SARS-CoV-2 peptide swimming pools. The researchers additionally measured T-cell immunodominance hierarchies and decided the potential for SARS-CoV-2 escape from T cell recognition via tradition enlargement.
Research findings
The primary COVID-19 wave in South Africa was dominated by the wildtype D614G pressure of SARS-CoV-2, whereas the second wave was dominated by the Beta variant. PBMCs have been utilized to guage the impact of HIV an infection on SARS-CoV-2 particular T-cell responses and decide T-cell cross-recognition.
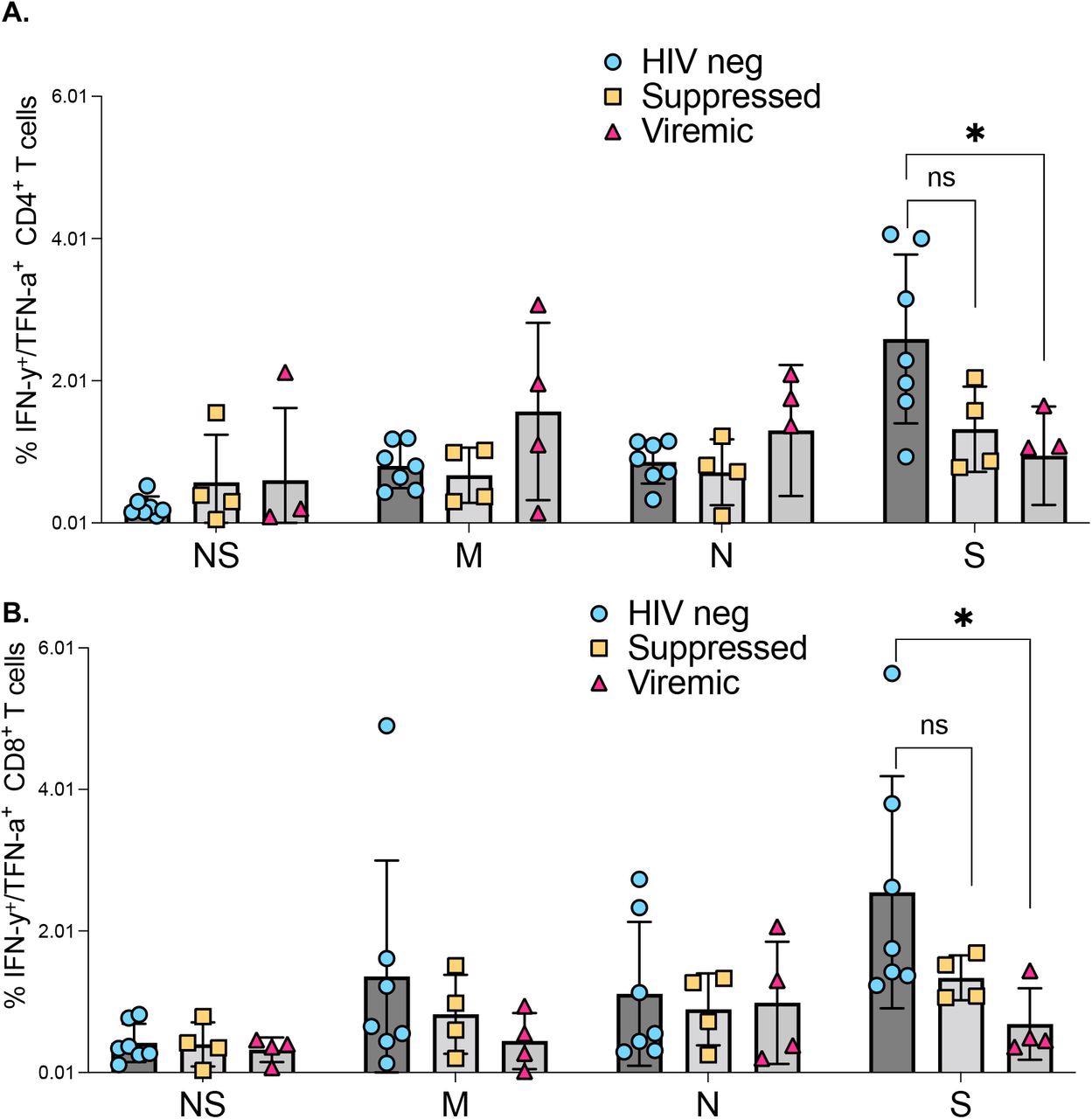
Comparability of SARS-CoV-2 protein concentrating on by T cell responses amongst HIV negatives, suppressed and viremic donors: The magnitude of (a) CD4+ T and (b) CD8+ T cell responses concentrating on SARS-CoV-2 proteins amongst examine teams. P-values for variations among the many teams are *<0.05; as decided by the Mann-Whitney U take a look at. (GraphPad Prism model 9.3.0)
Impaired SARS-CoV-2 particular T-cell responses have been recognized in people with unsuppressed HIV an infection. The researchers noticed a low rely of CD4+ T-cells, with hyperimmune activation, discovered to be associated to lowered SARS-CoV-2 particular T-cell responses.
The scientists additionally decided spike mutations within the Beta variant, which induced abrogate recognition by reminiscence T-cells raised towards epitopes of the unique SARS-CoV-2 pressure. Likewise, immune responses towards SARS-CoV-2 beta variant epitopes poorly cross acknowledged equivalent to authentic SARS-CoV-2 pressure epitopes, thus demonstrating the flexibility of sure SARS-CoV-2 variants to flee T-cell recognition.
People with unsuppressed HIV an infection have been discovered to exhibit poor responses to SARS-CoV-2 an infection. Moreover, HIV-induced immune defects akin to low CD4+ T-cell counts, increased HIV plasma viral hundreds, and elevated immune activation conferred lowered SARS-CoV-2 responses.
HIV-seronegative people exhibited strong CD4+ and CD8+ T-cell responses towards the SARS-CoV-2 spike protein in comparison with the PLWH. Moreover, lowered T-cell cross-recognition was noticed between the 2 COVID-19 waves, which was extra distinguished in individuals with unsuppressed HIV an infection.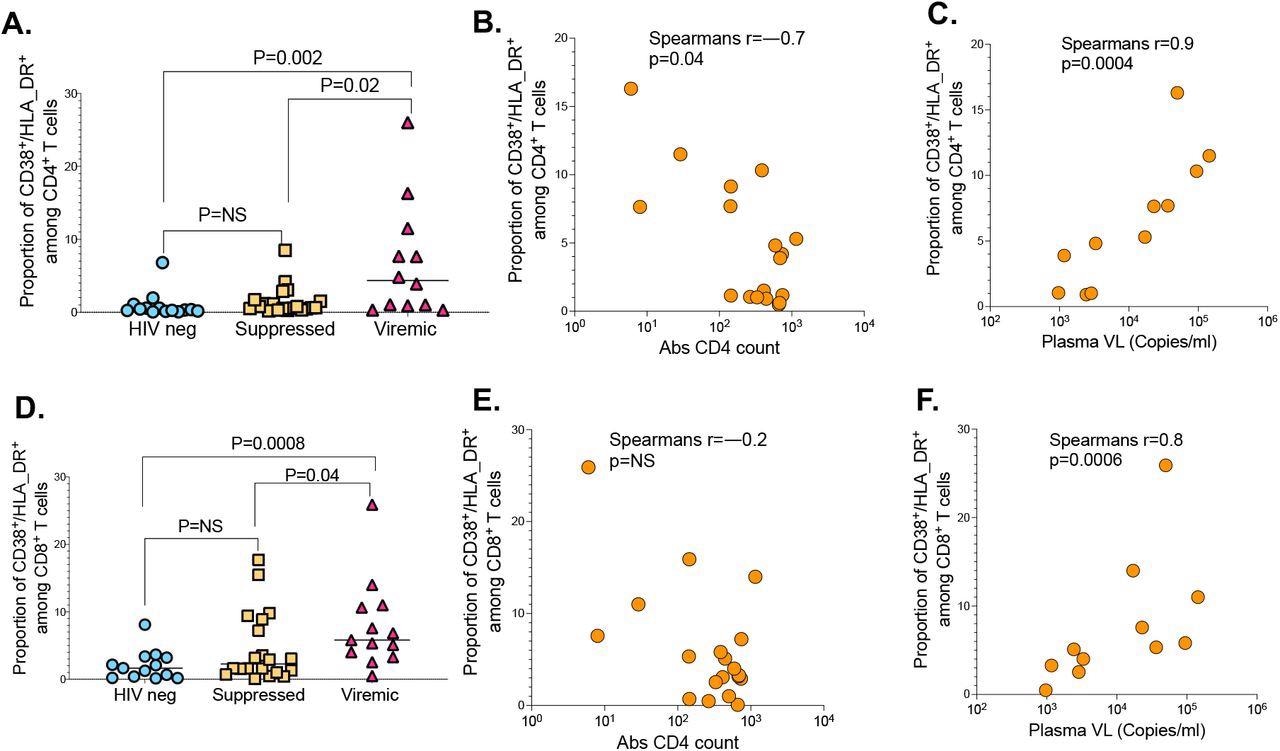
The influence of HIV markers of illness development on SARS-CoV-2 T cell immunity. (a) CD4+ T cell activation graphed based mostly on the frequency of CD38/HLA-DR co-expressing cells. (b) Correlation between CD4+ T cell activation and absolute CD4 counts. (c) Correlation between CD4+ T cell activation and HIV plasma viral load. (d) CD8+ T cell activation measured by CD38/HLA-DR. (e) Correlation between CD8+ T cell activation and absolute CD4 counts. (f) Correlation between CD8+ T cell activation and HIV plasma viral load.
conclusions
Unsuppressed HIV an infection considerably impairs T-cell responses to SARS-CoV-2 an infection and reduces T-cell cross-recognition. These findings clarify the elevated vulnerability of PLWH to extreme COVID-19, in addition to spotlight their susceptibility to an infection with rising SARS-CoV-2 variants.
*Vital discover
medRxiv publishes preliminary scientific stories that aren’t peer-reviewed and, subsequently, shouldn’t be thought to be conclusive, information scientific observe/health-related habits, or handled as established info.

